What are E-Prescriptions and How Do They Affect the Drug Problem?

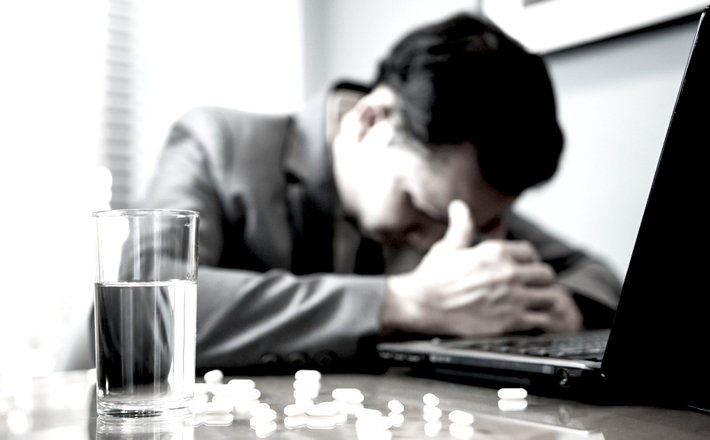
We are approaching a point in our society where drug and alcohol addiction are our primary concerns in the overall health and vitality of the American people. It is a terrible truth that drugs and alcohol would be the health conditions that we are most concerned about, but that is just the way it is. Our nation is struggling with terrible addition epidemics, crippling conditions of drug use with both legal and illegal drugs that affect tens of thousands of Americans.
According to the Substance Abuse and Mental Health Services Administration, there are currently twenty-four to twenty-five-million Americans who are addicted to drugs and alcohol. This is a greater total number of addicts than our country has ever had. It is also the most significant percentage of addicts per capita ever recorded in the United States.
Beginning in the 1990’s the United States saw a rise in the prescription and use of several new formulations of opioid painkillers. These new formulations, coupled with significant advertising and marketing to both physicians and patients created a perfect storm in which addiction grew to the unprecedented levels we see today.
Adding Technology to Our Traditional Systems is not Always Ideal
One of the most recent changes in the medical and pharmaceutical space has been an effort towards digitalizing the pharmaceutical drug prescribing process. Initially, this was to speed up and make the pharmaceutical prescribing process more effective and fluid. However, there is a fair degree of risk that comes along with digitalizing how doctors prescribe drugs, how patients fill their prescriptions, and how patients re-fill their prescriptions.
Because so many pharmaceutical drugs are dangerous and addictive and mind-altering, and because a vast percentage of prescription drugs carry with them severely adverse side-effects, doing anything with the prescribing process that could create errors in which patients get what drugs, how much they get, and in what dosage they get those drugs is something that we should all be very leery about. In fact, it might not be a good idea at all to take the prescribing process digital, to begin with.
There have already been too many overdose deaths, too many injuries and close-calls, all from patients who were not even addicts taking the wrong dosage or the wrong medication. And with how inventive and sneaky actual pill addicts are, the possibility for the manipulation of e-prescribing tools seems too great.
Expert Research Evaluations on E-Prescribing Software
In a direct quote from the U.S. National Library of Medicine, a department of the National Institutes of Health on the subject of electronic prescribing:
“Errors associated with the use of electronic prescribing have been slowly coming to light since the 2000s, as health care has become increasingly computerized. Serious adverse effects and even deaths have resulted from omissions, wrong-patient, wrong-drug or wrong-dose errors, and errors in drug administration…”

“Errors associated with the use of electronic prescribing have been slowly coming to light since the 2000s, as health care has become increasingly computerized. Serious adverse effects and even deaths have resulted from omissions, wrong-patient, wrong-drug or wrong-dose errors, and errors in drug administration. The use of order sets has led to duplicate therapy. Compared with handwritten prescriptions, the analysis of electronic prescriptions demands particular efforts on the part of pharmacists and other health professionals in order to detect errors.” (Source)
Obviously, there are some severe risks attendant with trying to switch opioid prescribing to a fully electronic and computerized system. For one, it takes the patient-doctor relationship out of the picture, diluting the sanctity and value of that relationship and the care-factor that doctors build with their patients over the years. That reason alone should be enough to turn down interest in e-prescribing. For another, the potential for abuse, error, and adverse effects in fully digitalizing the pharmaceutical prescribing process is more than a little bit prominent. Whatever gains in efficiency we garner out of this approach would be reneged due to the risks attendant with such systems.
The periodical, U.S. Pharmacist, also published a research paper on e-prescribing, specifically as pertains to community pharmacies. The research paper erred on the side of being neutral in as many instances as possible, but there was a note in their discussion as to the potential risks of such e-prescribing systems:
“In a recent study, one in 10 computer-generated prescriptions received by pharmacies had at least one medication error, and one-third of the errors were potentially harmful…”
“As with traditional prescriptions, errors associated with e-prescriptions are not always detected by the pharmacist, which can result in decreased safety, as well as patient harm. In a recent study, one in 10 computer-generated prescriptions received by pharmacies had at least one medication error, and one-third of the errors were potentially harmful. This is in contrast to previous reports suggesting that e-prescribing reduces preventable drug errors, thereby reducing patient harm. With such discrepancies, it is uncertain whether errors are decreased or increased with the use of e-prescribing software.”
Another article in Medical Economics also discusses the shortcomings of e-prescribing, discussing how the frailties in the proposed system simply leave too many loopholes and potentials for error in getting the right patients the right medicines. According to Sarah Corley, the chief medical officer of NextGen, one of the major companies that innovated e-prescription software:
“We get some pushback from physicians if they’re in an area where they get a lot of callbacks when they’ve sent something electronically and the pharmacist tells their patients, ’Your doctor didn’t send it,’ because the pharmacist didn’t look in the right place. That becomes frustrating, and then we have to try to work with the pharmacies in the area to make sure that they know what they’re supposed to be doing.” (Source)
This is only a handful of research data in the concerns and potential pitfalls of this new technology, but it is enough to shed concern on the potential risks we face with switching the doctor-patient prescribing approach to a fully electronic model.
Doctors Should See Patients More

From the above, selected research data, we can see that there is a great degree of controversy on the value or lack there-of of e-prescribing. And the above research data only touches on the tip of the iceberg on how dangerous e-prescribing could get. What’s next? Will doctors start seeing patients less and simply renew their patients’ prescriptions online?
The demand for doctors continues to grow as the population of doctors in active service, (about nine-hundred-thousand) continues to not increase in proportion to the increase in the American population. Doctors are already overwhelmed, so the projected appeal in seeing patients less and in handling prescriptions electronically might be a bit overpowering.
But this is the wrong direction to go in. If anything, we need our doctors to see their patients more. And we need doctors to be more hesitant to prescribe powerful and mind-altering drugs. We need doctors to push for alternatives to pharmaceuticals, especially when it comes to opioid pain relievers, psychotropic medications, and any other pharmaceutical drugs that pose a significant risk for abuse and misuse.
We need to create an American society where we prescribe drugs less, and where there is more interaction between doctors and patients, not less. Currently, prescription drugs account for the majority of the addiction epidemic, a grim fact that we all need to wake up to. If we can reduce our reliance on prescription drugs as a false “cure-all” for health problems, we will reduce the addiction problem considerably.
Sources:


 ®
®