Senior Citizens and Their Increasing Need for Addiction Recovery

No one deserves to die of a drug overdose, no one of any age whatsoever. When it’s a person in their 20s or 30s who succumbs, however, the loss might be as much of a shock. It’s not uncommon to get involved in risky activities when you’re young, including overuse of alcohol or use of addictive drugs. But when a person in advanced years lands in rehab or dies of an overdose, it’s downright confusing. Life isn’t supposed to work that way.
But it’s working that way now. Over the last couple of decades, more older adults are seeking treatment for problems with drug dependence. And more are suffering fatal overdoses.
It’s Not Just Alcohol Anymore
You might assume that most of these older adults seeking rehab are struggling with alcoholism. And you’d be right. However, the number of older adults needing rehab for alcohol is decreasing. Between 2000 and 2012, the percentage dropped from 77% to 64% of those entering rehab.
What are the drugs causing increases in the number of older adults seeking rehab?
- Cocaine and crack
- Marijuana and hashish
- Heroin
- Non-prescription methadone
- Other opioids
- Synthetic drugs
A Challenge: Managing Pain Among the Elderly

As we age, our bodies process painkillers and other drugs differently. We may not have as much ability to clear the drugs from our systems which means these drugs can accumulate to higher levels in our bodies than they would in a younger person. While doctors and dentists should adjust their prescribing as a person ages, it’s possible that not every practitioner will take this change into account.
Modifying prescriptions for painkillers or anti-anxiety drugs is of particular importance because of how often aging people receive prescriptions for these drugs. Why? Mostly for sleeping problems or pain.
Because of the common sleeping problems of older people, benzodiazepines or barbiturates may be prescribed. These drugs are all central nervous system (CNS) depressants which slow breathing and reduce brain activity. Their effects can help a person relax or sleep, but if the drug accumulates in an older person’s body, the effects could become life-threatening. Too much CNS depression and a person can stop breathing.
Seniors are also having more joint replacement surgeries than their younger counterparts. They receive more organ transplants and are more frequently diagnosed with cancer. Prescriptions for pain relievers—often opioids—are fairly inevitable. When the prescriptions continues over time, the likelihood of dependence increases. Only a few thousand doctors are trained in addiction medicine so your typical doctor may not realize when their patients become addicted or know how to wean patients safely off their medications if they do realize it.
Age and Alcohol
Just like with painkillers, our bodies process alcohol differently when we are older, meaning that the same amount of alcohol that was not life-threatening when we were young can result in dangerous impairment later in life. To this, add reduced body strength or balance problems and the result can be serious. Falls, burns or other accidents can result in injuries.
Aging brains and livers may be more severely affected by alcohol, prescription drugs, illicit drugs. A person could find themselves not recovering from drug or alcohol use as quickly, or liver or brain damage may intensify.

The CNS depression caused by alcohol may be more pronounced in later years. This means that an older person who drinks can be prone to these symptoms of CNS depression:
- Problems with movement or memory
- Slurred speech
- Lower blood pressure
- Poor concentration
- Dizziness
- Confusion
The family of an older person who drinks or uses prescription medication should be alert to the possibility that problems that might be ascribed to “just getting older” or cognitive decline are really from the use of alcohol or medications.
Combining Medications or Alcohol
Any substances that have a CNS-depressing effect are doubly dangerous when they are combined. Pain relievers and alcohol, for example. Or pain relievers and benzodiazepines, a very common combination. Older people are frequently on a combination of medications and they may not realize their cumulative effect. Or when they begin taking a medication, they may not realize that its effect could be magnified when they add their preferred alcoholic beverage.
To make matters worse, the confusion that results from CNS depression could make it impossible for an older person to work out the cause of any problems that result. That makes it vital for children and caretakers of older adults to know what they should be watching for.
Fatal Overdoses Among Mature Women
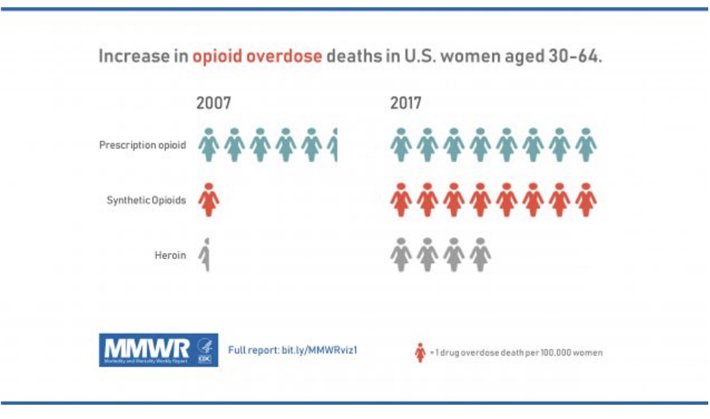
In 2019, the Centers for Disease Control and Prevention reported an increasing number of fatal drug overdoses among women between the ages of 30 and 64. The report noted increases in overdoses related to the use of benzodiazepines, cocaine, heroin, prescription opioids and synthetic opioids (mostly fentanyl).
In 1999, only 6.7 women per 100,000 population suffered fatal overdoses from opioids alone. By 2017, this number had risen to 24.3. The largest increases were seen in the 55 to 64 age group. Because individuals in this age group may not be suspected of drug dependence, their drug-related problems may be overlooked.
Between 2019 and 2020, the overdose death rate for both men and women rose sharply among those 45 to 54 years of age and the 55 to 64 group. There was a slight increase in those 65 and older.
Caring for an Aging Parent
Keeping older Americans free from addiction might require the assistance of their children or other caretakers. If a senior citizen is seeing more than one doctor, each practitioner may not be aware of all the prescriptions their patient is taking. It may be up to the family members to monitor the pills being prescribed and consumed.
That can mean anything from noting how many different practitioners are listed on pill bottles to counting the number of pills left in the bottles.
Of course, if the problem is with alcohol or a drug that is illicitly obtained, the monitoring duty must follow a different pattern. The responsibility may involve monitoring the person’s behavior, speech patterns or disabilities by asking yourself questions like these:
- Are they having more accidents or falls?
- Is their ability to walk or their strength diminishing?
- Is their speech less clear or coherent?
- Are they maintaining the same amount of interest in their favorite activities or family events?
- Are they sleeping more or not sleeping as well?
- Is their appetite the same, greater or less?
- Do they seem more secretive or moody?
- Do prescriptions come from more than one practitioner or pharmacy?
- Do they seem to require alcohol to relax or enjoy themselves?
The answers to these questions can point you in the right direction.
Addressing the Problem
In most cases, the first step should be a meeting with the individual and their primary care physician, bringing all medications along. If the problem is alcohol, bring along any information on the quantity of alcohol being consumed. From there, you can make a determination of what changes in their medication are called for, or if rehab is needed. As more older Americans need rehab, there will be more rehab facilities accustomed to the needs of these individuals.
Confronting a person with their growing dependence on alcohol, prescription medications or illicit drugs is never easy or pleasant. But it is a necessary task, whether it involves a teen, adult or senior. At any age, it can be the difference between an enjoyable life or a constant struggle, or even between life or death.
Sources:
- https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-017-2538-z
- https://www.usatoday.com/story/news/nation/2014/05/20/seniors-addiction-prescription-drugs-painkillers/9277489/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2546472/
- https://pubmed.ncbi.nlm.nih.gov/18090653/
- https://www.narconon.org/drug-abuse/alcohol/
- https://www.narconon.org/drug-abuse/barbiturate-signs-symptoms.html
- https://www.drugabuse.gov/publications/drugfacts/prescription-cns-depressants
- https://www.cancer.gov/about-cancer/causes-prevention/risk/age
- https://www.cdc.gov/mmwr/volumes/68/wr/mm6801a1.htm
- https://www.aamc.org/news-insights/21-million-americans-suffer-addiction-just-3000-physicians-are-specially-trained-treat-them
- https://www.nia.nih.gov/health/facts-about-aging-and-alcohol
- https://www.statista.com/statistics/611017/drug-overdose-deaths-number-in-the-us-by-age/
Reviewed and Edited by Claire Pinelli, ICAADC, CCS, RAS, LADC, MCAP, LCDC


 ®
®